Endometriosis Explained
Causes, Risk Factors, Diagnosis & Treatment
Endometriosis is a condition where tissue that normally lines the surface of the womb (called the endometrium) are found outside the womb. They respond to the same hormones that causes menstruation, leading to internal menstruation. The trapped blood irritates the area in which they are trapped, causing pelvic pain, heavy menses,very painful periods, pain during intercourse, and infertility. It is not cancer. It is not caused by an infection.
Endometriosis is a very common cause of severe painful periods, chronic unexplained abdominal pain, fatigue, exhaustion and sometimes, fertility problems in women between the ages of 20 and 50.
It does not occur before puberty, and tends to get better after menopause.
It is a condition that is difficult to diagnose.
The average time taken by doctors to make a firm diagnosis of this condition is 7 to 12 years from time of onset! Once the diagnosis is confirmed, it can be treated with the use of painkillers, the combined pill, hormones or surgery. It impacts significantly on the physical, emotional, mental and social wellbeing of suffers.
Many women with this condition are mistakenly treated as cases of pelvic inflammatory disease, irritable bowel syndrome, or anxiety.
Because this condition is treatable, it is important for any woman with chronic abdominal or pelvic pain that tends to be worse around the time of her menses or period, to be evaluated for endometriosis.
What Exactly is Endometriosis?

The word
endometriosis means spread of the endometrium (or lining of the womb) outside of
the womb to other parts of the body.
The endometrium has special cells and glands that are designed to grow and nourish a newly fertilized egg into a baby. Every month, this layer is shed off, if there is no pregnancy, in response to changes in the levels of oestrogen, the female hormone. This shed off endometrium tissue comes out as menstrual bleed. The endometrium is normally found only on the inner lining of the womb.
In endometriosis, this specialised tissue or groups of cells occur elsewhere.
This is abnormal.
They could be within the body of the muscle of the womb, on the floor of the pelvis, in the bowel, bladder, ovary, fallopian tube, skin, eyes, lung, kidney, or even rarely, in the brain!
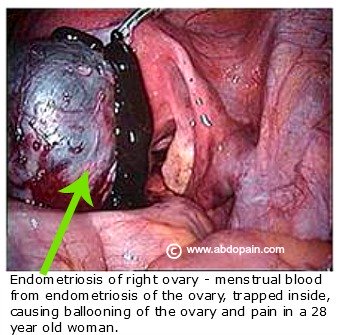
As the normal lining of the surface of the womb responds to changes in the level of hormones around the time of menstruation, these tissues outside the womb also respond to the hormones, leading to the accumulation of menstrual blood where the tissues exist. This trapped blood inside the woman cannot escape outside, unlike normal menstrual bled that escapes as menstruation.
The accumulated blood could cause distension, pain, scaring and sticking of organs or bowels together. That is why women with endometriosis tend to have more pelvic or abdominal pain around the time of their menses or period.
The body may absorb some of the blood over the next few weeks, until the next menstrual bleed, and the process continues.
What Causes Endometriosis?
Well, the truth is that we do not actually know exactly what causes endometriosis, or why some women have it and others don't.
What we do know however, is that it is a condition mostly found in western women. Certain behaviours and inheritance could increase the likelihood of developing endometriosis. Before discussing the behaviours or risk factors for endometriosis, the following explanations have been put forward as to why endometriosis occur:
- Retrograde Menstruation. Some experts belief that in some women, the lining of the womb shed during normal menstruation does not leave the body completely through the vagina and sometimes get sucked upwards instead of downwards, spreading backward into the tubes and ovaries to other organs and sites. They then get established outside in those ectopic sites, leading to endometriosis.
- Cell Transformation. Other experts contend that actually, the endometriotic cells found outside the womb are completely different in origin from those in the womb. They believe that in some women, the cells lining those areas where they develop endometriosis undergo sudden change in cell type in response to very high level of oestrogen hormones seen at puberty. They develop endometriosis due to a complex interaction between their genetic makeup, immune factors, and unique response to high levels of female hormones.
- Transfer Through Blood And Lymphatics. Those who support this theory think that actually, rather than through retrograde menstruation, normal tissues lining the wall of the womb sometimes "fall off" and gets carried through the veins from the womb and their lymphatic channels to other sites within or outside the pelvis. They call this the embolism theory.
- Surgical Implantation Theory. This is certainly a verified and established way in which endometriosis occurs. During surgeries like caesarean section or hysterectomy, the lining of the womb could be inadvertently cut and implanted outside the womb.
Risk Factors For Endometriosis
The following are risk factors for the development of endometriosis:
- Women who became pregnant after their mid twenties or have not been pregnant at all
- Women with short menstrual cycle
- Those with family history of endometriosis. You are 10 times more likely to have endometriosis if your sister, or mother is known to suffer with this condition
- Exposure
to endocrine-disrupting chemicals like dioxin exposure (caused endometriosis in
79% of monkeys in one study!)
- Use of certain type of vinyl and plastics in microwave oven (leads to the release of chemicals that causes hormone imbalance
- Use of pesticides
- Presence of auto-immune disease like MS (multiple sclerosis), lupus and rheumatoid arthritis.
While endometriosis tends to get better after menopause, there is a form of endometriosis that occurs in post-menopausal women called Postmenopausal endometriosis. It is an aggressive form of this disease and it is characterised by complete progesterone resistance and extraordinarily high levels of the hormone, aromatase.
Smoking
reduce endometriosis by inducing early menopause by 1.5-3 years, depending on how long you've smoked.
Some Startling Statistics About This Condition
- You may be surprised to know that endometriosis is so common. This condition is believed to be present in as many as one in every ten women. Over 2 million women in the UK and 6 million in the USA suffer with endometriosis.
- 80 percent (8 out of 10 women) with chronic pelvic or lower abdominal pain are due to endometriosis.
- About 40 percent of women who develop endometriosis do so following caesarean section
- 50 percent of women undergoing fertility investigation will have evidence of endometriosis.
- If treated, this condition could come back again within a 5 year period in 20 to 40 percent of patients.
What Are The Symptoms Of Endometriosis
The symptoms of endometriosis depend more on where it is. In most cases, it causes no symptoms at all. This condition causes symptoms only when there is significant accumulation of menstrual blood or irritation, scaring and adhesion.
The classical patient with endometriosis will complain of:
- Dull
continuous lower abdominal pain every time, but worse near to during or shortly
after their menstrual period. The pain may spread to the lower back too as a dull annoying ache.
- They may experience deep seated pelvic pain during intercourse and such pain tend to be worse just before or after their menses
- There may be lower abdominal pain on passing urine or opening one's bowel, worse around the time of menstruation
- Upper thigh or leg pain (sciatica) at about the same period every month
- There may be blood stain or passage of blood in your urine or stool from time to time around the time of menstruation
- Difficulty in conceiving or achieving pregnancy in association with any of these symptoms listed here
- Feeling fatigued or exhausted for no apparent reason in combination with any of the above symptoms
- Pain on an old caesarean section scar, even many months or years after the operation, that tends to be worse around the time of menstruation.
Other Conditions That May Mimic Endometriosis
The symptoms of endometriosis can also be mimicked by other conditions including:
- Irritable bowel syndrome
- Pelvic Inflammatory Disease
- Pelvic Adhesions
- Interstitial cystitis
- Ovarian cyst or tumour
Each of the above conditions can be excluded by a detailed attention to the pattern of pain and carrying out specific tests to confirm the diagnosis.
How Is Endometriosis Diagnosed?
The diagnosis of endometriosis is from a careful history or story given by the patient, combined with certain tests to confirm the diagnosis.
If you have:
- Severe period pain
- Pain during intercourse
- Difficult to diagnose long standing lower abdominal pain,
Your doctor might request the following tests:
- Ultrasound scan of your abdomen and pelvis. This
test may come back as normal, because ultrasound scan can only pick up
significant collections of fluids or cysts if the ovary is distended by
endometriosis (referred to as chocolate cyst), or deep seated endometriosis inside the bulk and muscle of the womb called adenomyosis.
- Laparoscopy. This is how endometriosis is confirmed. Laparoscopy is the use of a camera attached to the end of a small tube to look directly inside the pelvis. By means of a laparoscope, the doctor would be able to see the endometriosis directly and even take some samples for laboratory testing.
- MRI. Sometimes, there may be need to use an MRI instead of laparoscopy in the diagnosis of endometriosis.
Treatment
If you are confirmed to have endometriosis, do not despair. At least now you know what has been causing you those terrible pain that no one else seem to understand. It can be treated. Actually, you don't have to treat it, if it is not causing you any trouble. If you decided to go for treatment, your choice of treatment should be guided by:
- Your age - if you are young in your 20s and 30s, you may decide to go for a gentler medical, rather than surgical treatment if possible
- Effect on your fertility, if any or whether you have already completed your family
- The extent of the disease and its effect on you
- Type of treatments you have had in the past for this condition, if any and their effect on you
- Affordability, if you do not have medical insurance
It is important to know that:
- In many
cases, this condition is not curable. Most treatment only suppresses symptoms or
reduce the bulk of the disease. The only hope for cure is through a radical surgical operation where the womb, fallopian tubes and ovaries are removed, with the destruction and removal of all visible disease.
- Endometriosis will clear and disappear on its own without any treatment in 1 in 3 women; become worse and deteriorate in 50 percent of women with this disease if nothing is done; and will remain exactly the same in the other third of women.
The treatment options that exist for endometriosis include:
Do nothing. This is an option to consider if the condition is an accidental finding without any symptoms, and fertility is not affected and if you are not keen to take medications or undergo surgery yet.
Medical Treatment. This is the option almost everyone starts with. Note that with medical treatment, symptoms may come back within 6 to 12 months of completion of treatment. Medical options available for the treatment of this condition include:
- Use of Painkillers. This basically involve the use of Non-Steriodal Anti Inflammatory Drugs like ibuprofen to control pain and inflammation. Diclofenac used to be a popular option, but recent evidence linking the use of diclofenac to increased risk of heart disease has lead to reduced use of this agent. Naproxen is another alternative, if ibuprofen is not helpful. Also, you can add paracetamol (Tylenol) and codeine to the use of NSAIDS in pain control.
- Hormonal Drugs. These are the main stay of treatment for this condition. Hormonal drugs are used for about 6 to 9 months to help reduce pain. The mostly used hormonal medicines are the combined contraceptive pills, danazole, gestrinone and GnRH agonist (eg Triptoreline acetate - also called Decapeptyl SR, 3mg injection, once every month for 3-4 months). In women who cannot use the combined contraceptive pill, a progesterone, Medroxyprogesterone acetate at a dose of 10 mg three times a day, starting from the first day of their menses for 90 or more days has been shown to effectively control symptoms.
- Mirena Coil. The use of Mirena intra-uterine system (IUS) has been shown to both reduce endometriosis growth outside the womb and help to achieve pain reduction.
Surgical Treatment. Because no hormone treatment offers the prospect for complete cure, many women would need surgery in addition to medical treatment. Surgical options available and what they aim to achieve include:
- Laparoscopy for Diagnosis & Removal of Endometriosis Deposit. This is the most basic and common surgical intervention for this condition. During keyhole or laparoscopic surgery to confirm the diagnosis of endometriosis, any deposit seen could be burnt off with a laser beam. It is very effective for pain control and reduce the bulk of disease. This can be the first step if you do not like the idea of trying hormones. Laparoscopic surgical treatment can be done as a day case surgery and you will be ready to go home that same day.
- Radical Surgery. If you have a severe form of endometriosis with disabling symptoms, radical surgery could be an option for you. This is even more so if you have completed your family and do not think you would ever want more kids. This kind of surgery involves the complete removal of the womb (hysterectomy), fallopian tubes, and the ovaries, as well as any vestige of endometriosis deposit seen in the pelvis. If both ovaries are removed, you will no longer be able to produce the female hormone oestrogen that causes endometriosis to grow. You will need to be on HRT. The small amount of oestrogen in HRT will be too small to cause resurgence of endometriosis.
Complementary And Alternative Treatments.
There are many complimentary therapies that have been used in combination with medical or surgical treatment of endometriosis.
Though there are no scientific evidence to support the benefit of some of these alternative or "natural remedies for endometriosis", they are worth considering to see if they will work for you. No doctor should dismiss their use completely. Be sure to be safe in whatever you do in this regard.
Complementary treatments for endometriosis available include:
- Nutritional Therapy. This involve the use of certain food items, vitamins and supplements in the treatment of endometriosis. Foods recommended and believed to be good for endometriosis include beans, lentils, broccoli, cherries, avocados, cashew nuts and fish rich in omega3 fatty acids.
- Acupuncture. There a number of published reports to show that acupuncture has been used to successfully treat the pain of endometriosis. You may want to speak with a certified acupuncture practitioner in this regard.
- Homeopathy. The homeopathic medicines, Graphites, Lachesis and Oophorinum has been used with varying success in the treatment of endometriosis.
- Natural Herbs. There are claims that a number of Western and Chinese herbs offer some relief from the pain and symptoms of endometriosis, when taken as per the prescription of practitioners experienced in this field.
References:
- Endometriosis - Suspected. Map of Medicine Ltd. 14th March 2012
- Endometriosis: What You Need To Know. Royal College of Obstetricians and Gynaecologists. Published November 2007
- Endometriosis. Obstetrics and Gynaecology. A Core text with self-assessment. By Andrew McCarthy And Bill Hunter. Published 1998. Pages 160 - 162.
Last Updated:
18th September 2013.
Endometriosis: Have Your Say!
Do you have an experience or story about endometriosis? Or are you suspecting that this condition might be the cause of your monthly abdominal pain? We would love to hear from you! Have your say here now.
If you think you might have endometriosis, why not contact our online doctor by providing the following information here as well as a brief summary of your medical history:
- Describe the pain you have
- How long exactly have you been experiencing this pain for (months, years etc)?
- Where on your abdomen is the pain - e.g at the level of bikini line?
- What have you noticed makes the pain worse?
- What makes it better - eg pain killers or use of water bottle, or rest or lying still or nothing?
- Does the pain tend to be worse around the time of your period or menses, if so how many days to your period or after?
- Do you also experience pain when using the loo or restroom? If so where exactly is this pain?
- Is there any pain during intercourse, if you are sexually active?
- How bad is your pain ... on a scale of 1 to 10?
- How is this affecting your life, work and relationship?
- When did you start your very first period - how old were you then and how many days does your period flow for?
- Do you have any problems trying to conceive, and if so, for how long now?
- What do you use for contraception, if anything?
- Is there anyone in your family that has been firmly diagnosed with endometriosis?
What Other Visitors Have Said
Click below to see contributions from other visitors to this page...
Sticth like pain for 3days on right side of stomach Not rated yet
I have had a constant stitch like pain for 3-4 days now. It just above the right side of my hip in my abdomen and also server lower back pain. I have …
pain on the right side of my navel Not rated yet
My name is Marie 33 years, I had three successful c-section but like after a year or two i started having pain on the right side of my navel, at first …
abdominal pain unexplained Not rated yet
unexplained abdominal pain in my lower right side for about 3 years it comes and goes, i have have ct scans, colonoscopy, and my appendix out but they …
the week before my period starts, i have intense pain deep in my right hip socket and lower abdomen Not rated yet
Hi there, 24 year old female. I have been experiencing pain in my lower abdomen for a few months now along with some other symptoms.
I was diagnosed …
painful abdomen low down and swollen tummy Not rated yet
for 4 months very low down in my abdomen I have had a constan dull ache that can be quite painful and doesnt go away. Also I have experienced a sharp stabbing …
|
Help Keep This Site Going |

Return From Endometriosis - An Overview, To Causes Of Lower Abdominal Pain