Pathophysiology of Appendicitis
Pathophysiology of appendicitis refers to the processes that occur in a normal appendix that eventually lead to the development of appendicitis. Simply put, it actually refers to the sequence of events that causes appendicitis and the natural history or natural progression that occurs once an appendix becomes inflamed. A knowledge of the pathophysiology of acute appendicitis no doubt is helpful in understanding how swift the condition should be handled, should the diagnosis of appendicitis be suspected.
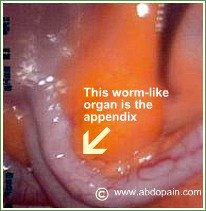
The appendix was once thought to be a "vestige" or remnant tissue in our gut that has no use. It is only in the last few years that a better understanding of the function of the appendix has developed.
It has been demonstrated that the appendix, unlike its closest neighbor, the colon, contains numerous clusters of special type of white blood cells called B and T lymphoid cells. These clusters of special white blood cells also called "lymphoid tissue" are part of our immune or defense systems in the gut that mediates immunologic function to protect the body from invasion by harmful organisms.
Appendicitis occurs when this wall of defense - the lymphoid system is overwhelmed.
It used to be believed that all acute appendicitis results from swelling and lumen obstruction of the appendix and subsequent proliferation of bacteria or viruses, leading to the disease. That view is changing.
Appendicitis has now been classified into three types based on the histology and process leading to inflammation of the appendix.
The three types of appendicitis are:
- Mucosal Appendicitis. This is the mildest form appendicitis. It results from inflammation and superficial ulceration of the mucosa of the appendix without involvement of the whole wall of the organ. It is often seen in very early appendicitis where the organ - that is, the appendix may look normal and non-inflamed to the naked eye but certainly demonstrates several superficial erosive and hemorrhagic lesions and surrounding inflammatory infiltrates on histology. Mucosal appendicitis is usually diagnosed at histology only.
- Phlegmonous Appendicitis. This is an inflamed appendix with pus or abscess formation. It is a slow to develop process and it's clinical progress is often slow too. A phlegmonous appendix is believed to be the stage resulting from mucusal obstruction and subsequent bacterial colonization.
- Necrotic Appendicitis. A necrotic appendix is often due to acute bacteria invasion of the appendix with loss of blood supply, leading to rapid damage of the wall of the appendix and perforation. This is the most severe form of appendicitis, as delay in identifying and treating this type of appendicitis could lead to the discharge of feces into the abdominal cavity with widespread dissemination of bacteria in the abdominal cavity leading to rapid death from sepsis.
Once these different types of appendicitis is understood, the pathophysiology of appendicitis becomes clear. Understanding the pathophysiology of acute appendicitis also helps to explain all the signs and symptoms as well as complications seen in appendicitis. We shall now explain the processes that typically occur with the development and progress of appendicitis.
Step By Step Explanation of The Pathophysiology of Appendicitis And How it Relates to The Clinical Picture.
One of the main thrust of events leading to the development of acute appendicitis lies in the appendix developing a compromised blood supply due to obstruction of its lumen and becoming very vulnerable to invasion by bacteria found in the gut normally.
Obstruction of the appendix lumen could occur from a number of things, leading to a rise in intra-luminal pressure, which causes the wall of the appendix to become distended.
Things that could block the lumen of the appendix leading to the process of appendicitis include:
- Faecolith (a fecolith is a small masses of feces, calcium salt, bacteria and shredded lining of the wall of the bowel forming a stone hard object)
- Enlarged lymph node or lymphoid tissue
- Intestinal worms like Ascaris lumbricoides or Pin worms (Enterobius vermicularis) reaching the appendix from the small intestines or colon
- Tumour - like carcinoid tumours
- indeed foreign objects - like sand grains or maize or other objects that got into the appendix from ingested food.
Normal mucus secretion continues within the lumen of the appendix, thus causing further build up of intra-luminal pressures. This in turn leads to the occlusion of the lymphatic channels, then the venous return, and finally the arterial supply becomes undermined.
Reduced blood supply to the wall of the appendix means that the appendix gets little or no nutrition and oxygen. It also means little or no supply of white blood cells and other natural fighters of infection found in the blood would be vailable to the appendix.
The wall of the appendix will thus, start to break down and rot. Normal bacteria found in the gut gets all the inducement needed to multiply and attack the decaying appendix within 36 hours from the point of luminal obstruction, worsening the process of appendicitis.
This leads to necrosis and perforation of the appendix. Pus formation occurs when nearby white blood cells are recruited to fight the bacterial invasion.
A combination of dead white blood cells, bacteria, and dead tissue makes up pus.
The content of the appendix (faecolith, pus and mucus secretions) are then released into the general abdominal cavity, bringing causing peritonitis.
In some cases, this perforation could be sealed off by omentum, leading to contained appendiceal abscess with less rapid deterioration seen in the patient.
So, in acute appendicitis, bacterial colonization follows only when the obstruction and cutting off of the blood supply of the appendix occurs. The early stage of this process is what is seen in mucosal appendicitis.
These events occur so rapidly, that the complete pathophysiology of appendicitis takes about one to three days. This is why delay can be deadly!
- Pain in appendicitis is thus caused, initially by the distension of the wall of the appendix, and later when the grossly inflamed appendix rubs on the overlying inner wall of the abdomen (parietal peritoneum) and then with the spillage of the content of the appendix into the general abdominal cavity (peritonitis).
- Fever is brought about by the release of toxic materials (endogenous pyrogens) following the necrosis of appendicael wall, and later by pus formation.
- Loss of appetite and nausea follows slowing and irritation of the bowel by the inflammatory process.
The pathophysiology of appendicitis obviously correlates with the clinical picture.
Acute appendicitis pathophysiology follows the same pattern, even in children and pregnant women.
In the elderly, the pathophysiology of appendicitis remains unaltered, but the inflammatory response generated by the elderly is often less than that seen with young fit individuals, accounting for the often benign presentation froth with a tendency to missing the diagnosis, thus courting more complications.
Published on October 4th 2007 by Abdopain.com Editorial Team under causes of right sided lower abdominal pain.
Article was last reviewed on 11th October 2015.
References:
- Mulholland, MW, Lillemoe, KD, Doherty, GM, et al. Greenfield's Surgery, 4th ed, Lippincott Williams & Wilkins, Philadelphia, PA 2005
- Gut and liver 06/2011; 5(2):234-7. DOI:10.5009/gnl.2011.5.2.234 · 1.81 Impact Factor
- http://www.uptodate.com/contents/acute-appendicitis-in-adults-clinical-manifestations-and-differential-diagnosis
- http://oxfordmedicine.com/view/10.1093/med/9780199699476.001.0001/med-9780199699476-chapter-7
Appendicitis Stories - Have Your Say!
Are you suffering with a right sided abdominal pain? Do you suspect that this might be due to appendicitis? Or have you had your appendix removed? What was your experience like? Share your appendicitis stories here. We would really love to hear from you!